Northern Ontario's state of Mental Health and Why
August 18, 2020 - According to the Government of Canada, mental health is defined as a state of psychological and emotional well-being. Good mental health is extremely important for individuals and for society. It allows one to live happily, achieve maximum productivity, and to better cope with life’s challenges. Poor mental health can lead to mental and physical illness, which is why it is crucial that communities implement services that foster good mental health. In this blog, we will first explore the state of mental health in Northern Ontario. Next, potential explanations for Northern Ontario’s state of mental health will be provided.
Self-reported mental health has been found to be a good indicator of mental health and well-being. So let’s compare the percentage of individuals that perceived their mental health as good or excellent for each of Northern Ontario’s seven health units (Figure 1). All health units in Northern Ontario - except for the North Bay and Parry Sound District Health unit – had a lower percentage of individuals that perceived their mental health as very good or excellent compared to Ontario for the year 2017-2018 (Figure 1).
Figure 1
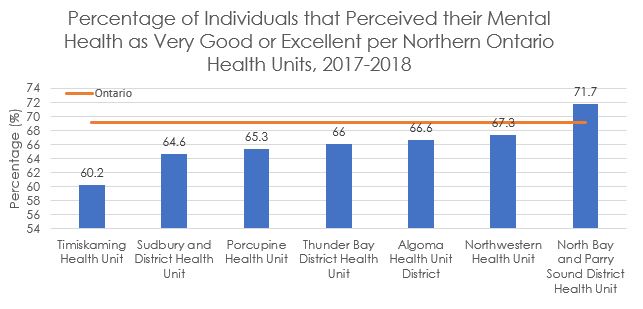
Source: Statistics Canada. Table 13-10-0113-01. Health characteristics, two-year period estimates.
One potential explanation for the lower perceived mental health in Northern Ontario may be lack of access to care. Mental health services are less accessible in rural areas and Northern Ontario is largely rural or remote. Previous analysis has demonstrated that costs associated with travelling to neighbouring urban regions deter individuals from receiving important mental health services.
When comparing the Local Health Integration Networks (LHIN) discharge rates[1] per 100 000 people for hospitalizations in the mental health and addictions category, the numbers are much higher for the North East and North West LHINs (Figure 2)2,3. Mental illness and addictions are significant issues in Northern Ontario. This would obviously contribute to the lower perceived mental health state outlined in figure 1.
The lack of mental health services provided by primary health care teams, centres for addiction and mental health, and other counselling groups would compound this problem. In the absence of community mental health services individuals with mental health and addictions must visit hospitals as their primary access point for receiving help. Creating a higher percentage of hospital intakes for the northern LHINs but also undercounting those in need of service in rural and remote areas with no hospital access.
Figure 2
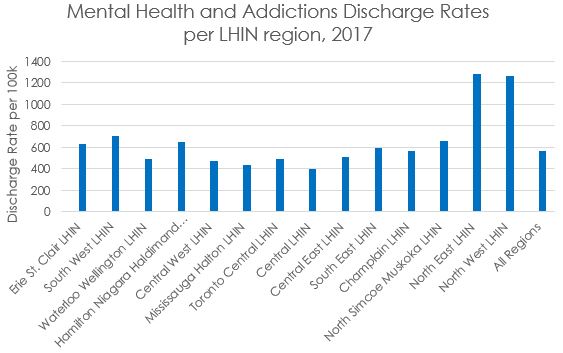
Source: Canadian Institute of Health Information. Mental Health and Addictions Hospitalizations in Canada, by Health Region.
Poor mental health does not necessarily mean someone has a mental illness. The social determinants of mental health can help explain the low percentages in individuals reporting very good or excellent mental health in Northern Ontario. Important determinants of mental health are social inclusion, freedom from discrimination and violence, and access to economic resources. The community well-being index is measured by combining data on income, education, housing and labour force activity. The average community well-being index using census data from 1981 to 2006 and 2016 and 2011 National Household Survey data was 69.6 in Northern Ontario compared to 74.9 for Ontario overall. As such, the lower levels of socio-economic well-being reported in Northern Ontario may play a role in self-perceived mental health that fares worse compared to the rest of Ontario. On the other hand, social inclusion is unlikely to be an important factor for Northern Ontario since all, but the North Bay and Parry Sound District Health Unit had higher rates of self-reporting a strong sense of belonging to their community (Figure 3).
Figure 3
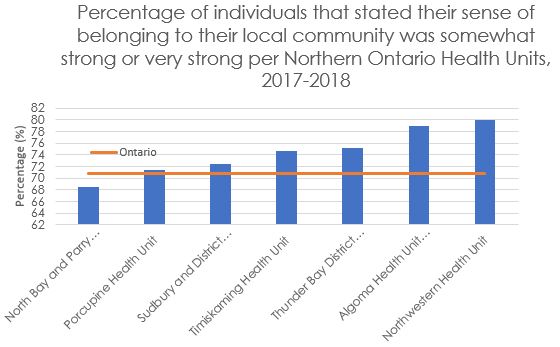
Source: Statistics Canada. Table 13-10-0113-01. Health characteristics, two-year period estimates.
Northern Ontario also has a significantly different demographic compared to the rest of Ontario. According to the 2016 census, 2.8 percent of the Ontario population self-identified as an Indigenous person whereas Northern Ontario had a much larger proportion with 18.4%[1]. The percentage of Indigenous peoples (excluding reserves) in Canada aged 18 and older that reported excellent or very good mental health was 60% for First Nations, 64% for Métis and 53% for Inuit. In comparison, 72 per cent of the non-Indigenous Canadian population reported excellent or very good mental health. It is very likely that intergenerational trauma from colonization and historical discriminatory policies in Canada like residential schools and the Indian Act created the conditions that fostered this observed health inequity between Indigenous and non-Indigenous peoples.
Francophones make up 18.8% of the Northern Ontario population compared to 4.7% of the Ontario population[2]. It is unclear whether the Francophone demographic of Northern Ontario contributes to the lower mental health outcomes, because Francophone self-perceived mental health data is unavailable. However, Francophones in a community where they are a linguistic minority might have differential access to healthcare resources and mental health support services. Using micro survey data from the Canadian Community Health Survey , 38% of francophones that declared living in a linguistic minority situation stated suffering from mental illness compared to 34% in Canada. It is important to ensure communities that have francophone linguistic minorities have access to French health services because language influences perceptions of health, relationships with health professionals/counsellors and their knowledge on health services and other possible resources.
Potential solutions are being attempted in Northern Ontario to improve access to Mental Health services. Telemedicine is becoming more utilized throughout Ontario, which suggests that this can increase access to psychiatric services. However, communities lacking internet access cannot benefit from this service. In 2008, 8 out of 14 Family Health Teams in Northern Ontario had at least one mental health professional within their interdisciplinary team. Having more mental health professionals incorporated in family health teams may improve patient care and well-being in the community. Visiting psychiatrists through the Ontario Psychiatric Outreach Program is another way to improve access to mental health services in rural and remote Ontario. However, the 2008 survey of family health teams reported that the lack of continuous and consistent care from having different psychiatrists at each visit hinders the quality of the patient’s care.
Different combinations of these solutions should be implemented locally in Northern Ontario communities in a personalized manner given the needs and resources of the community. Monitoring and evaluation should also be conducted to determine if adjustments improved the mental health and well-being of its people.
[1] Author’s calculation: Beyond 2020 Aboriginal Target Group Profile
[2] Author’s calculation: Beyond 2020 Francophone Target Group Profile
[1] Standardized for age
2 Local Health Integration Networks are non-profit agencies funded by the Ministry of Health and Long-Term Care to plan, fund and integrate health services for their local communities.
3 Mental health and addictions discharge rate is defined as the number of patients whose recorded primary diagnosis or the diagnosis that contributed most to their hospital stay at discharge falls under a mental health or addictions category for a defined year.
Write for us
Maia Kvas is a Research Analyst at NPI
Thank you to our Experience North Sponsor 
The content of Northern Policy Institute’s blog is for general information and use. The views expressed in this blog are those of the author and do not necessarily reflect the opinions of Northern Policy Institute, its Board of Directors or its supporters. The authors take full responsibility for the accuracy and completeness of their respective blog posts. Northern Policy Institute will not be liable for any errors or omissions in this information, nor will Northern Policy Institute be liable for any detriment caused from the display or use of this information. Any links to other websites do not imply endorsement, nor is Northern Policy Institute responsible for the content of the linked websites.
Northern Policy Institute welcomes your feedback and comments. Please keep comments to under 500 words. Any submission that uses profane, derogatory, hateful, or threatening language will not be posted. Please keep your comments on topic and relevant to the subject matter presented in the blog. If you are presenting a rebuttal or counter-argument, please provide your evidence and sources. Northern Policy Institute reserves the right to deny any comments or feedback submitted to www.northernpolicy.ca that do not adhere to these guidelines.
